Physical Function Tracking

Physical Function Tracking
Monitoring Physical Function Following Acute Hospitalization
Longitudinal Tracking for Post Hospitalization Outcomes
Funded by The Center on Health Services Training and Research - CoHSTAR

Visit CoHSTAR
On this page
Acute hospitalization, particularly for older adults, can have profound and persistent consequences on physical function. 1,2 Many studies have reported declines in physical function during and after an acute hospital stay with functional deficits persisting at least a year following hospitalization. 3–5 Sustained deficits in physical function are an important risk factor for several adverse post-hospitalization outcomes.
Inconsistent assessment of physical function has hampered our ability to learn what interventions ought to be implemented to maximize physical function across the continuum of care settings.
Our long-term goals
- Define a process for consistent physical function data collection beginning in the acute hospital and following patients as they proceed to post-acute care settings and return to community living
- Create a place for those data to be shared and used for understanding and improving long-term changes in physical function.
Our team, with representatives from University of Utah Health, Johns Hopkins Medicine, and the Cleveland Clinic received pilot funding to help define a standard data tool kit for longitudinal tracking of physical function from acute care hospitalization through post-acute care settings and into the community. Defining the tool kit involved facilitating consensus from key stakeholders including rehabilitation therapists, case managers, discharge planners, registered nurses, administrators, patients and a core group of experts.
The purpose of this website is to share the current tool kit with other interested health systems and individuals and to provide a mechanism for discussion and input. This tool kit represents a first step in standardizing a minimum set of data to collect in the inpatient and home health settings only. We anticipate including other care settings in the future.
Have feedback or questions?
'
Minimum Data Set
Administrative data
Data routinely collected and documented in the electronic health record; collected only one time.
| Hospital Admission Data | Demographic | Post Hospital |
| Unique Patient identifier | Age | Discharge date |
| Payer | Race | ICU stay (Y/N) |
| Admission date | Sex | ICU length of stay |
| Zip code | Body mass index | Hospital length of stay |
| Principal diagnosis | Ethnicity | Discharge medication list |
| All ICD 10 | Hospital discharge disposition | |
| PT/OT/SLP utilization | ||
| 30 day all cause readmission (Y/N) | ||
| Death (Y/N) | ||
| Procedure codes (CPT) | ||
| MS-DRG | ||
| Case mix index | ||
| Surgery (Y/N) | ||
| Deep vein thrombosis | ||
| Hospital acquired pressure injury III or IV | ||
| Hospital acquired pressure injury (any) | ||
| Hospital acquired pneumonia | ||
| Injurious falls (#) |
Provider collected data
Data collected by a health care provider. Collected at one time only. In order to minimize burden we are recommending using common, standard questionnaires and patient reported outcomes currently available and often required by regulatory bodies. Most are available at no or low cost.
The Continuity Assessment Record and Evaluation (CARE) Item Set Questions (B1, B3, B3a, B5a-e, B6, B7)
- Prior to this hospitalization, where did the patient live?
- Private Residence
- Community based residence (e.g., assisted living residence, group home, adult foster care)
- Long term care facility (e.g., nursing home)
- Other (e.g., shelter, jail, no known address)
- Unknown
- If the patient lived in the community prior to this illness, what help was used?
- No help received or no help necessary
- Unpaid assistance
- Paid assistance
- Unknown
- If the patient lived in the community prior to this illness, who did the patient live with?
- Lives alone
- Lives with paid helper
- Lives with other(s)
- Unknown
- Indicate the patient’s usual ability with everyday activities prior to this current illness, exacerbation or injury (Use the following to score – 1. Independent, 2. Needs Some Help, 3. Dependent, 4. NA, 5. Unknown)
- Self-Care (Did the patient need help bathing, dressing, using the toilet or eating?)
- Indoor Mobility - Ambulation (Did the patient need assistance with walking from room to room (with or without devices such as cane , crutch or walker)?)
- Indoor Mobility – Stairs (Did the patient need assistance with internal or external stairs (with or without devices such as cane , crutch or walker)?)
- Indoor Mobility – Wheelchair (Did the patient need assistance moving from room to room using a wheelchair, scooter, or other wheeled mobility device?)
- Functional Cognition (Did the patient need help planning regular tasks such as shopping or remembering to take medication?)
- Mobility devices or aids used prior to hospitalization
- Cane/crutch
- Walker
- Orthotics/prosthetics
- Wheelchair/scooter full time
- Wheelchair/scooter part time
- Mechanical lift
- Other (specify)_________________________
- None apply
- Unknown
- History of falls prior to hospitalization – Has the patient had two or more falls within the past year or any fall with injury in the past year?
- Yes
- No
- Unknown
Other – collected daily or at each visit
| Acute Hospital | Home Health |
| AM-PAC mobility – 6 clicks | AM-PAC mobility – home health |
| AM-PAC activity – 6 clicks | AM-PAC activity – home health |
| Johns Hopkins Highest Level of Mobility | |
| CAM ICU – if appropriate | |
|
Pain Interference – OASIS (M1242) Frequency of Pain Interfering with patient's activity or movement: a) Patient has no pain b) Patient has pain that does not interfere with activity or movement c) Less often than daily d) Daily, but not constantly e) All of the time
|
Pain Interference – OASIS (M1242) Frequency of Pain Interfering with patient's activity or movement: a) Patient has no pain b) Patient has pain that does not interfere with activity or movement c) Less often than daily d) Daily, but not constantly e) All of the time
|
| Cognition – intact, mild impairment, > mild impairment (instrument of choice) | Cognition – intact, mild impairment, > mild impairment (instrument of choice) |
Instruments
The Activity Measure for Post Acute Care (AM-PAC)
Confusion Assessment Method for the ICU (CAM-ICU)
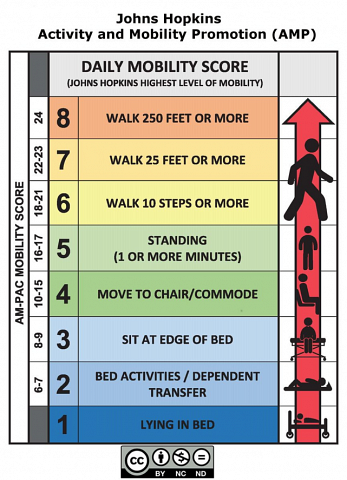
Johns Hopkins Highest Level of Mobility (JH-HLM)
JH-HLM Mobility Goal Calculator
Johns Hopkins Daily Mobility Goal Calculator
Johns Hopkins Highest Level of Mobility Score AM-Pac Mobility Score
8 – Walk 250 feet or more 24
7 – Walk 25 feet or more 22-23
6 – Walk 10 steps or more 18-21
5 – Standing (1 or more minutes) 16-17
4 – Move to chair or commode 10-15
3 – Sit at edge of bed 8-9
2 – Bed activities/dependent transfer 6-7
1 – Lying in bed --
Resources/References
- Ahasic AM, Van Ness PH, Murphy TE, Araujo KLB, Pisani MA. Functional status after critical illness: agreement between patient and proxy assessments. Age Ageing. 2015;44(3):506-510. doi:10.1093/ageing/afu163.
- Allen J, Hutchinson AM, Brown R, Livingston PM. Quality care outcomes following transitional care interventions for older people from hospital to home: a systematic review. BMC Heal Serv Res. 2014;14:346. doi:10.1186/1472-6963-14-346
- Bierman AS. Functional status: The sixth vital sign. J Gen Intern Med. 2001;16(11):785-786. doi:10.1046/j.1525-1497.2001.10918.x.
- Bogasky S, Kline T, Kelleher C, Lines LM, Coots L, Garfinkel D. Analysis of Crosscutting Medicare Functional Status Quality Metrics Using the Continuity and Assessment Record and Evaluation (CARE) Item Set Assessment Record. Washington, DC; 2012.
- Boyd CM, Landefeld CS, Counsell SR, et al. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc. 2008;56(12):2171-2179. doi:10.1111/j.1532-5415.2008.02023.x.
- Brown CJ, Friedkin RJ, Inouye SK. Prevalence and Outcomes of Low Mobility in Hospitalized Older Patients. J Am Geriatr Soc. 2004;52(8):1263-1270. doi:10.1111/j.1532-5415.2004.52354.x.
- Burke RE, Whitfield EA, Hittle D, et al. Hospital Readmission From Post-Acute Care Facilities: Risk Factors, Timing, and Outcomes. J Am Med Dir Assoc. 2016;17(3):249-255. doi:10.1016/j.jamda.2015.11.005.
- Centers for Disease Control and Prevention, National Hospital Discharge Survey. 2010.https://www.cdc.gov/nchs/nhds/index.htm. Accessed August 31, 2017.
- Centers for Medicare & Medicaid Services. The Inpatient Rehabilitation Facility - Patient Assessment Instrument (IRF-PAI) Training Manual. 2012. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS/Downloads/IRFPAI-manual-2012.pdf. Accessed September 27, 2017.
- Chambers MA, Moylan JS, Reid MB. Physical inactivity and muscle weakness in the critically ill. Crit Care Med. 2009;37(10 Suppl):S337-S346. doi:10.1097/CCM.0b013e3181b6e974.
- Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51(4):549-555. https://www.ncbi.nlm.nih.gov/pubmed/12657078
- Colla CH, Lewis VA, Bergquist SL, Shortell SM. Accountability across the Continuum: The Participation of Postacute Care Providers in Accountable Care Organizations. Health Serv Res. 2016;51(4):1595-1611. doi:10.1111/1475-6773.12442
- Daley KN. Adding power to systems science in rehabilitation. Physical Therapy. 2018;98(8):725-726.
- de Villiers L. Frailty is often the final stage of life and needs to be recognised and managed appropriately. Contin Med Educ. 2013;31(10):353-357.
- Ehlenbach WJ, Larson EB, Randall Curtis J, Hough CL. Physical Function and Disability After Acute Care and Critical Illness Hospitalizations in a Prospective Cohort of Older Adults. J Am Geriatr Soc. 2015;63(10):2061-2069. doi:10.1111/jgs.13663.
- Frontera WR, Bean JF, Damiano D, et al. Rehabilitation Research at the National Institutes of Health: Moving the Field Forward (Executive Summary). Am J Phys Med Rehabil. 2017;96(4):211-220. doi:10.1097/PHM.0000000000000700.
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322-1327.
- Glasgow RE, Kaplan RM, Ockene JK, Fisher EB, Emmons KM. Patient-Reported Measures Of Psychosocial Issues And Health Behavior Should Be Added To Electronic Health Records. Health Aff. 2012;31(3):497-504. doi:10.1377/hlthaff.2010.1295
- Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, Restricted Activity, and the Development of Disability Among Older Persons. JAMA. 2004;292(17):2115. doi:10.1001/jama.292.17.2115.
- Haley SM, Coster WJ, Andres PL, et al. Activity Outcome Measurement for Postacute Care. Med Care. 2004;42(Supplement):I-49. doi:10.1097/01.mlr.0000103520.43902.6c.
- Hoyer EH, Young DL, Klein LM, et al. Toward a Common Language for Measuring Patient Mobility in the Hospital: Reliability and Construct Validity of Interprofessional Mobility Measures. Phys Ther. 2018;98(2):133-142. doi:10.1093/ptj/pzx110
- Hoyer EH, Needham DM, Atanelov L, Knox B, Friedman M, Brotman DJ. Association of impaired functional status at hospital discharge and subsequent rehospitalization. Journal of hospital medicine : an official publication of the Society of Hospital Medicine. 2014;9(5):277–82. doi:10.1002/jhm.2152
- Hoyer EH, Needham DM, Miller J, Deutschendorf A, Friedman M, Brotman DJ. Functional Status Impairment Is Associated With Unplanned Readmissions. Archives of Physical Medicine and Rehabilitation. 2013;94(10):1951–1958. doi:10.1016/j.apmr.2013.05.028
- Hoyer EH, Young DL, Klein LM, et al. Toward a Common Language for Measuring Patient Mobility in the Hospital: Reliability and Construct Validity of interprofessional Mobility Measures. Phys Ther. November 2017. doi:10.1093/ptj/pzx110
- Hoyer EH, Young DL, Friedman LA, et al. Routine Inpatient Mobility Assessment and Hospital Discharge Planning. JAMA Intern Med. November 2018. doi:10.1001/jamainternmed.2018.5145
- Integrated Treatment for Co-Occurring Disorders Evidence-Based Practices (EBP) KIT|SAMHSA.https://store.samhsa.gov/product/ Integrated-Treatment-for-Co-Occurring-Disorders-Evidence-Based-Practices-EBP-KIT/SMA08-4367. Accessed September 27, 2017.
- Jackson JC, Pandharipande PP, Girard TD, et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med. 2014;2(5):369-379. doi:10.1016/S2213-2600(14)70051-7.
- Jenq GY, Tinetti ME. Post–Acute Care: Who Belongs Where? JAMA Intern Med. 2015;175(2):296. doi:10.1001/jamainternmed.2014.4298
- Jette AM. Toward Systems Science in Rehabilitation. Phys Ther. 2016;96(3):270-271. doi:10.2522/ptj.2016.96.3.270
- Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM. AM-PAC “6-Clicks” functional assessment scores predict acute care hospital discharge destination. Phys Ther. 2014;94(9):1252-1261. doi:10.2522/ptj.20130359
- Johnson JK, Fritz JM, Brooke BS, et al. The Association Between Patients’ Physical Function in the Hospital and their Outcomes in Skilled Nursing Facilities. PTJ-PAL. 2019;19(4):5-16.
- Johnson JK, Erickson JA, Miller CJ, Fritz JM, Marcus RL, Pelt CE. Short-term functional recovery after total joint arthroplasty is unaffected by bundled payment participation. Arthroplasty Today. 2018. doi:10.1016/j.artd.2018.12.003
- Kansagara D, Englander H, Salanitro A, et al. Risk Prediction Models for Hospital Readmission. JAMA. 2011;306(15):1688. doi:10.1001/jama.2011.1515.
- Krumholz HM. Post-hospital syndrome—an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100-102. doi:10.1056/NEJMp1212324.
- Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332(20):1338-1344. doi:10.1056/NEJM199505183322006.
- Li J, Brock J, Jack B, et al. Project ACHIEVE - using implementation research to guide the evaluation of transitional care effectiveness. BMC Heal Serv Res. 2016;16:70. doi:10.1186/s12913-016-1312-y
- Linstone, Harold A. and Turoff M. The Delphi Method: Techniques and Applications. Boston, MA: Addison-Wesley; 1975.
- Menezes KVRS, Auger C, Barbosa JFS, Gomes CS, Menezes WRS, Guerra RO. Trajectories and Predictors of Functional Capacity Decline in Older Adults From a Brazilian Northeastern Hospital. J Geriatr Phys Ther. December 2019. doi:10.1519/JPT.0000000000000255
- Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: The importance of transitional care in achieving health reform. Heal Aff. 2011;30(4):746-754. doi:10.1377/hlthaff.2011.0041
- Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10(1):53. doi:10.1186/s13012-015-0242-0.
- Saliba D, Jones M, Streim J, Ouslander J, Berlowitz D, Buchanan J. Overview of significant changes in the Minimum Data Set for nursing homes version 3.0. J Am Med Dir Assoc. 2012;13(7):595-601. doi:10.1016/j.jamda.2012.06.001.
- Sandel ME, Jette AM, Appelman J, et al. Designing and implementing a system for tracking functional status after stroke: a feasibility study. PM R. 2013;5(6):481-490; quiz 490. doi:10.1016/j.pmrj.2012.09.579
- Shaughnessy PW, Crisler KS, Schlenker RE. Medicare’s OASIS: Standardized outcome and assessment information set for home health care. Home Healthc Now. 1996;14(7):547-548.
- Siebens H, Andres PL, Pengsheng N, Coster WJ, Haley SM. Measuring physical function in patients with complex medical and postsurgical conditions: a computer adaptive approach. Am J Phys Med Rehabil. 2005;84(10):741-748. http://www.ncbi.nlm.nih.gov/pubmed/16205429.
- Wald HL, Ramaswamy R, Perskin MH, et al. The Case for Mobility Assessment in Hospitalized Older Adults: American Geriatrics Society White Paper Executive Summary. Journal of the American Geriatrics Society. 2018;0(0). doi:10.1111/jgs.15595
- Wells M, Williams B, Treweek S, Coyle J, Taylor J. Intervention description is not enough: evidence from an in-depth multiple case study on the untold role and impact of context in randomised controlled trials of seven complex interventions. Trials. 2012;13(1):95. doi:10.1186/1745-6215-13-95.
- Wu X, Li Z, Cao J, et al. The association between major complications of immobility during hospitalization and quality of life among bedridden patients: A 3 month prospective multi-center study. PLOS ONE. 2018;13(10):e0205729. doi:10.1371/journal.pone.0205729
- Young DL, Colantuoni E, Friedman LA, et al. Prediction of Disposition within 48-hours of Hospital Admission Using Patient Mobility Scores. J Hosp Med. 2019;14:E1-E4. doi:10.12788/jhm.3332
Provide Input
If you have feedback or questions please contact Robin Marcus at
robin.marcus@hsc.utah.edu